The Playground Bully Inside Your Nervous System
Never is harmony more important than inside the human body. Every biologic process depends on a delicate balance. Actions that can be turned on, must also be able to be turned off. Things that are sped up should be able to be slowed down. When dealing with the central nervous system, this balance becomes particularly important. The reason for this is that the central nervous system is the foundation that runs every other cell, organ and system inside of your body. For instance, it controls your sleep, immune system, hormones, healing, as well as pain levels. The central nervous system is composed of the brain and the spinal cord. I always tell my patients to think of the nervous system as the foundation of the body. If it is flawed or malfunctioning in any way, every other part of the body will be affected.
It is very important, when trying to understand how the human body works, to realize and appreciate how integral the central nervous system is to the body. When an embryo develops, the nervous system is the first to differentiate or form. It is the system that runs the entire body. It controls every single function or task that your body performs. If the brain is the captain; the spinal cord is the highway that carries the signals and commands to every cell and delivers feedback to this captain. It is the master control system. Every feeling of discomfort or pain involves the nervous system. In order for you to be healthy, this system has to be healthy.
The Autonomic Nervous System
In this blog, we take a closer look at the autonomic (or automatic) nervous system. While I don’t need you to become an expert on neurology (who has the time?), I do want to make sure that you have a good basic understanding of how this system works and what it controls (everything!) so that many of the mysterious neurological symptoms associated with CRPS will make sense. When you understand how something started going haywire in the first place, you can begin the process of fixing it.
Typically, our current health care system consists of managing symptoms. This can be done in many different ways. Nerve signals of pain and discomfort are seen as a bothersome and unwanted symptom and may be numbed or interrupted. Nerves may be removed. Organs will also often be removed. If a part hurts, it must be silenced, numbed, or taken out. Today, this way of thinking has become normal for most of us.
What I am about to say may sound extreme, but I stand by it. Unless the body is in an extreme emergency situation where immediate action is needed to prevent permanent damage, organ loss, or death, medical management of symptoms rarely contributes to longevity or improved health, and most often may actually take away from the patient’s overall quality of life. Please note that under some circumstances, such as Parkinson’s, symptom management is very understandable and appropriate. However, generally speaking, symptom management should preferably be exercised only for limited periods of time.
All that being said, it’s understandable why CRPS sufferers desperately reach for relief in the form of a pill, spinal cord stimulator, or infusion. Anything, anything to put out the fire. It is impossible to function in everyday life while in excruciating pain. However, such management of pain should never be confused with a healing process or improved health. Please note that I do not judge anyone who suffers from CRPS who needs pain relief. My hope is simply for you to find the answers that will make it possible for you to live without daily pain medication.
Let’s take a closer look at the autonomic nervous system and how it causes some of the most common symptoms associated with CRPS.
The autonomic nervous system is a control system within your peripheral and sensory nervous system that influences the function of internal organs. This system acts largely automatically without any conscious input from you and regulates bodily functions such as digestion, sexual arousal, respiration, heart rate, blood pressure, and urination to name a few. Certain reflex actions such as sneezing, coughing and vomiting are also controlled by the autonomic nervous system. Within the brain, the autonomic nervous system is controlled by the hypothalamus. The hypothalamus is located just above the brain stem within the brain.
This system is divided into the sympathetic and parasympathetic nervous system. The sympathetic nervous system is largely responsible for speeding up functions in the body, and is known as the “fight or flight” system. The parasympathetic nervous system is considered the “rest and digest” or “feed and breed” nervous system, and mostly is responsible for slowing functions down inside the body. Think of the sympathetic nervous system as the gas pedal in your car, and of the parasympathetic nervous system as the break.
The One Thing Every Single CRPS Patient’s Nervous System Has In Common
What if your body was an airplane and your pilot drunk? The autonomic nervous system (sometimes known as the automatic or involuntary nervous system) is incredibly important to your health, as this system is the master control system that runs every single function in your body. Most of these functions require no conscious thought from you. You don’t have to remember to breathe, for example. When you are sitting in an airplane, you don’t have to know exactly what the pilot is doing up there in the cabin. You just trust that he is doing his job and will keep the plane in the air and eventually land it safely. In the case of most CRPS sufferers, the pilot is unfortunately up to all sorts of monkey business, and usually has his hand frozen in the full-throttle position.
The sympathetic and parasympathetic nervous systems have exactly opposite effects on the functions of the body. They essentially work in opposition to each other, but in a way that complements each other. As I said earlier, think of your sympathetic nervous system as the gas pedal, and the parasympathetic nervous system as the brake pedal. The balance between the two is crucial for the perfect function of every cell in your body. While they are both crucial to the car, they cannot be stepped on at the same time.
In every single CRPS patient, the sympathetic nervous system has its pedal to the metal, all the time. This may be the case years before you ever develop CRPS, or your nervous system may be injured resulting in this imbalance when you suffer from the traumatic injury that triggered your CRPS. As many CRPS sufferers, unfortunately, find out firsthand, this is bad news for your health. The golden rule of the autonomic nervous system is that if one system is up, the other system must be down.
The Sympathetic Nervous System: “Fight or flight”
This system was designed to help your body fight to stay alive when your survival is being threatened. Think of a caveman in hand-to-paw combat with a saber-toothed tiger. This portion of your nervous system responds very quickly (think zero to ninety in a few seconds), since one usually doesn’t have time to calmly ponder one’s response to a life-threatening situation. When your life is being threatened and your body gets ready to fight in order to ensure its survival, every small bit of energy spent is carefully considered. Nothing is wasted. Energy will be rerouted away from systems that do not concern themselves with short-term survival, to where it can be used more readily to fight an immediate threat. For example, blood will flow away from the digestive tract and skin in order to be rationed out to the lungs and muscles. It is more important under those circumstances to be able to fight using your muscles and to breathe hard and fast, as your body needs oxygen.
Speaking of oxygen, the bronchioles (small air passages) in the lungs will open up, which allows for more oxygen into the blood. At the same time, the heart will beat faster. Another physiological change in the body is that the pupils will dilate, allowing more light to enter the eyes. The adrenal glands on top of the kidneys will pump adrenalin in case you need extra motivation besides fear to fight. It will also make all the sphincters (think of pressure valves) in the body, like the urinary sphincter, contract and close tight.
So why does this affect you? There probably isn’t the equivalent of a saber-toothed tiger chasing you every day. Your brain cannot distinguish fear and stress from actual life-threatening situations. Additionally, as mentioned earlier in this book when we discussed emotional stress, a very old traumatic event can run in a continuous “loop” in the subconscious mind. The brain cannot distinguish between this old memory and present danger. The old memory almost acts like a computer virus, messing with the software in your nervous system. Your brain does not know that it isn’t happening anymore.
When a person suffers an emotionally traumatic event or a neck injury following, for example, a fall or car accident affecting the brainstem directly or indirectly, the sympathetic nervous system will become overexcited, affecting the whole body.14,15,16 This will cause your sympathetic nervous system, or “fight or flight” response, to be stuck in the “on” position day in and day out—and if your sympathetic nervous system is stuck all the time, your parasympathetic nervous system is turned off. Instead of these two systems working in perfect harmony, the sympathetic nervous system turns into the schoolyard bully, or the puppet master, pulling your body’s strings and directing it on a disastrous course every second of the day. This will create the perfect conditions inside your body that put you at risk to develop CRPS and other autonomic dysfunction or WAD (whiplash-associated dysfunctions). I will discuss each symptom in detail, after we explain how the parasympathetic nervous system works.
The Parasympathetic Nervous System: “Rest and Digest” or “Feed and Breed”
Think of your parasympathetic nervous system as the system that calms you down, helps you to rest and sleep, helps to facilitate healing in the body and deals with sexual arousal. It functions to counter the sympathetic system. After a crisis or danger has passed, this system helps to calm the body. Your heart and breathing rates slow, your digestion resumes, your pupils contract, and you stop sweating.
This system will also cause the increase of blood flow to your GI tract following a meal to allow digestion. It stimulates the movements of your intestines (called peristalsis) that move food through your intestines. It will constrict the pupil of the eye, cause you to salivate when appropriate, and is responsible for getting you in the mood for sex. This system, if activated, will activate your immune system, cause increased circulation to the skin and extremities, and help to release your “feel-good” hormones, called endorphins. It will also decrease temperature. It is the main control system that promotes healing. This system is usually underactive, suppressed, or turned off in those who suffer from CRPS. No wonder you are not in the mood for getting frisky!
The Vagus Nerve: Your Severed Lifeline
If you suffer from CRPS, you should familiarize yourself with the Vagus nerve, as it is a major player in building the puzzle that forms CRPS. The Vagus nerve is the single most important nerve inside the human body outside of the spinal cord. It is one of twelve pairs of cranial nerves. These nerves emerge directly from the brain and brainstem, as opposed to spinal nerves that emerge from the sides of the spinal cord. Each cranial nerve is paired and is present on both sides. The cranial nerves provide motor and sensory information mainly to the structures of the head and neck (think sensations like smell, taste, hearing, or vision, for example.) These nerves are numbered by Roman numerals. The Vagus nerve is the tenth nerve (CN X), and it is the longest cranial nerve.
Please stick with me here, as I realize that some of you may be bored by the anatomy of the nervous system. I promise that this nerve matters greatly in the development (and therefor also the healing) of the neurological symptoms of CRPS.
The Vagus nerve (meaning “wandering nerve”) has multiple branches that diverge from two thick stems rooted in the cerebellum and brainstem that wander to the lowest viscera of your abdomen also connecting to your heart and most major organs along the way, such as the lungs. The Vagus nerve supplies motor parasympathetic fibers to ALL the organs except the adrenal glands, from the neck down to the transverse colon. The Vagus nerve is responsible for many different tasks, including (but not limited to): heart rate, digestion, sweating, speech, coughing, fainting, and vomiting, to name but a few. Remember, people who suffer from CRPS also suffer from sympathetic dominance (the schoolyard bully), causing the parasympathetic nervous system to be suppressed and to shut down. This means that people who suffer from CRPS also suffer, by definition, from an underactive Vagus nerve.
Just to recap: the parasympathetic nervous system is responsible (in general) for slowing and calming things down, as well as healing and sleep. The Vagus nerve forms an electric circuit that links our heart, digestive tract, and lungs to the brain. Let’s look at how this nerve affects specific organs just a bit closer.
Your Achy Breaky Heart
In a normal heart, the resting heart rate is controlled by the parasympathetic nervous system. It has been shown that the resting heart rate (meaning your heart rate when you aren’t engaged in physical activity) is a measure of your Vagus nerve function and predicts mortality. The Vagus nerve also controls inflammation in the body. For now, I did want to mention, however, that Vagus nerve suppression will lead to inflammation of the tissue of the heart, causing tissue injury, preventing remodeling of cells, and leading to cell death. Vagus nerve stimulation, in turn, will prevent tissue injury and cell death in the heart17,18.
The higher the Vagus nerve activity is, the greater the increase in the parasympathetic component of heart rate variability is, the slower your heart rate is, and the better the outcome is. In people who suffer from heart failure, heart rate is less regulated by parasympathetic activation. There is a clear relationship between increased heart rate and adverse outcomes, such as heart failure.
CRPS patients are particularly vulnerable to cardiac disease and malfunction. While no specific study has been performed to link the incidence of cardiac disease and CRPS, it is my belief that such a link does exist.
Just Breathe: How The Vagus Nerve Affects Your Lungs
The Vagus nerve is one of the key players that help you to breathe and keep your lungs healthy. When the lung expands during normal breathing, the Vagus nerve sends a message to the brain that causes the bronchi to constrict. We cannot survive without oxygen for more than 5 minutes. Therefor, breathing is essential not only to our health, but to our very survival. There is an undeniable link between an overactive immune system, inflammation, and breathing disorders such as asthma, COPD (Chronic Obstructive Pulmonary Disease) and sleep apnea19. Sleep apnea is actually very common amongst people who suffer from Fibromyalgia and CRPS. When you are not breathing correctly, it will also affect your sleep at night, which in turn affects healing. Healing happens much more effectively during deep, quality REM sleep than your waking hours.
In addition, proper breathing is very vital to maintain the health of your brain and Central Nervous System. During relaxed abdominal breathing, your brainwaves will also show a pattern of relaxation. The Vagus nerve uses a neurotransmitter called acetylcholine that communicates with the diaphragm which is essential for breathing.
It is interesting that not only does the Vagus nerve help to regulate your breathing, but you can activate the Vagus nerve in return by using specific breathing, namely slow, deep breaths, breathing from the abdomen, and exhaling longer than you inhale. When we think of breathing, we tend to focus on oxygen only. The truth is that breathing serves other functions as well. Exhaling carbon dioxide is actually a powerful detoxification pathway in the body. We literally breathe out our waste (hence morning breath). When our lungs are not doing so effectively, we overburden our other detoxification pathways, such as the kidneys and liver.
When the lungs expand and contract it has an effect on the body that is almost like a pumping action, much like the heart, but bigger. It is responsible for tissue repair, lymphatic drainage of waste products, activation of the immune system, and dilation of blood vessels which is crucial for healing, to name but a few.
Gut Feelings Are Actually Real: How the Vagus Nerve Connects With Your Emotions.
The Vagus nerve is constantly sending real time sensory information about the body’s organs to your brain via nerves called afferent nerves, meaning, leading into the brain. Efferent nerves, in turn, lead out of the brain. About 90% of the nerve fibers in the Vagus nerve are dedicated to communicating the state of your organs to your brain every nanosecond.
Gut instincts are not imaginary, but are actual emotional signals transferred to your brain via the Vagus nerve. Signals from the Vagus nerve traveling from your gut to your brain have been linked to changes in your mood and emotions such as fear and anxiety. Underlying these gut feelings is a little known network of neurons lining our guts like tiny fingers that is so sophisticated that some call it our second brain. These nerves are filled with neurotransmitters and does much more than merely controlling digestion. This second brain (called the enteric nervous system) in our insides, together with the brain in our heads, help to determine our emotional state and also play a key role in certain diseases throughout the body.
Although its influence is far-reaching, the second brain is not the seat of any conscious thoughts or decision-making. The enteric nervous system contains about 100 million neurons, more than in either the spinal cord or the peripheral nervous system put together. It consists of sheaths of interconnected neurons embedded in the walls of the long tube of our gut, which measures about twentynine feet from the esophagus to the anus. The enteric nervous system enables our brain to be in touch with the inner world of our gut, although it is not capable of rational thought, such as putting together a shopping list.
A big part of our emotions is influenced by the nerves in our gut. Butterflies in the stomach, which is a typical stress response, is one example of this. The enteric nervous system uses more than 30 neurotransmitters, just like the brain, and in fact about ninetyfive percent of the body’s serotonin is produced in the gut. Depression has been shown to be directly linked to abnormalities in the gut, affecting serotonin levels20.
Jeepers Creepers: How Unhealthy Gut Bacteria Control You And Your Habits
Inside our gut live millions of bacteria, some good, and some bad, together weighing about as much as our brain. When we are healthy, the good bacteria far outweigh the bad. The Vagus nerve can actually alert our brain if this balance is tipped towards the unhealthy bacteria if it is functioning correctly. If we are unhealthy, the bad can overcome the good in numbers, leading to dire consequences. Much like people, different bacteria need different foods in order to thrive. Some prefer fats, and some prefer sugar. Some even recognize and are repulsed by the supplements that may kill or harm it. While it is unclear exactly how this occurs, it has been shown that this diverse community of bacteria, collectively known as the gut microbiome, may influence our decisions by releasing signaling molecules into our gut. It is almost as if we have millions of little aliens in our guts.
Because the gut is linked to the immune system, the endocrine system and the nervous system, those signals could influence our physiologic and behavioral responses as well as our choices of, for example, the food we eat. In other words, the bugs in our gut manipulate us to pick the foods that they prefer. They will also release unpleasant chemicals in our blood when we take a supplement or eat foods that can kill them. This is why the supplements or foods that your body sometimes needs the most will physically repulse you. Microbes will also affect our mood and emotional state. Microbes have the capacity to manipulate behavior and mood by altering the neural signals in the vagus nerve, producing toxins to make us feel bad, and releasing chemical rewards to make us feel good.
Fortunately, you are still in control of our own body, and you can evict these toxic little unwanted squatters. How? You can actually use food to kill off bad bugs in our gut and do so fast. As a matter of fact, as soon as you change your eating habits, changes can be measured within as early as twenty- four hours. For this reason, we will cover diet and supplementation in more detail later in this book.
Leaky Gut And Allergies
Patients who suffer from intestinal disorders, such as a leaky gut, will often develop allergies. What exactly is a leaky gut? This should be of interest to you, as the majority of CRPS patients suffer from it. Normally, the intestinal lining forms a barrier between all the stuff we eat and our blood. This protects our bodies and also filters needed nutrients from unwanted ones. The small intestine is designed to allow very small particles of digested nutrients to pass through its wall and into the bloodstream, where it is distributed throughout the body as needed.
Due to a variety of causes, the intestinal wall can become more permeable or “leaky” and allow larger, half-digested food particles or toxins and waste to pass through, causing what is known as leaky gut syndrome. The cause of this may be decreased nervous system communication to the gut, resulting in “bad housekeeping” and damage to the gut, which is most often the case in CRPS. Other possible causes may be chronic inflammation, using the birth control pill, chronic emotional stress, food sensitivities, a sluggish liver, damage from taking large amounts of nonsteroidal anti-inflammatory drugs (NSAIDS), medications, radiation or certain antibiotics, excessive and long-term alcohol, caffeine, or tobacco use, too much sugar, heavy metal toxicity, candida overgrowth, or decreased immunity.
When these particles enter the bloodstream, the immune system recognizes them as foreign invaders and attempts to fight them off. Over a long period of time, this will cause your immune system to malfunction and may result in autoimmune conditions and allergies. The first step in treating leaky gut syndrome and other GI problems in a CRPS patient should be restoring proper nervous system communication to the GI system, as discussed elsewhere in this book.
When Eating Becomes Torture: The Vagus Nerve And Your Digestive System
One of the symptoms that is pretty universal in all CRPS patients, besides pain, is digestive issues. These issues will be varied, depending upon the patient and how long they have been sick. In its mild first stages, patients usually suffer from indigestion, heartburn, constipation and/or diarrhea, and bloating. As it progresses, patients may suffer from food allergies, leaky gut syndrome, Crohn’s disease, and chronic inflammation of the GI tract. In its most severe form, patients will suffer from gastroparesis, or weakness (paralysis) of the muscles of the stomach.
The Vagus nerve helps manage many complicated processes in your digestive tract, including signaling the muscles in your stomach to contract and push food into the small intestine. A malfunctioning Vagus nerve can’t send signals to your stomach muscles. This results in poor digestion of the food in your stomach, and the slowing down of the emptying of your stomach. Patients who suffer from this condition will have a very difficult time ingesting anything other than liquids. This condition results in nausea, vomiting, and severe abdominal pain. CRPS patients suffering from GI problems are usually treated like patients with two separate conditions, rather than a patient with a central nervous system malfunction resulting in both conditions. The distinction here is an important one, as one treatment approach works, and the other doesn’t.
Medical treatment of GI problems usually involves prescribing medication(s) to manage symptoms (for instance to force the bowels to function more regularly) and under very extreme circumstances, surgery to remove malfunctioning parts. Diet is seldomly addressed, and even when it is addressed, it is done so poorly. Managing symptoms without addressing the root cause is like putting a wet towel over a fire alarm while the house is burning down. Not only is this approach not helpful, it is actually harmful. In order to tackle this problem logically, you must first understand why the GI system started malfunctioning in the first place.
Sleep, A Distant Memory
This quote reminds me of CRPS patients: “Remember when you woke up all refreshed after going to bed early and drifting off to sleep easily? Me either.” Besides the constant pain, sleeping problems are probably one of the most annoying and life-robbing symptoms CRPS patients suffer from.
Sleeping serves a very important function. While you are sleeping, your nervous system has much more energy available for healing. There are many reasons for this. During this time, you are not thinking. Thinking invariably evokes emotions, which requires some of your available energy to be spent. Your senses are, for the most part, shut down. You are not hearing, seeing, or smelling. You are not using your large muscle groups to move around. All the energy normally used on these functions can now be redirected and used to assist your body in the healing process. However, if you are sleep-deprived, your body is missing out on this golden opportunity. It is estimated that your body heals about three times faster while asleep. It is a cruel twist of fate that the patients who need this most are the very patients who can’t sleep.
Sleep problems with CRPS include insomnia or difficulty falling asleep as well as waking up frequently. An even more common problem is frequently waking up even though you don’t remember doing so the next day, which interrupts your “deep” sleep. Also, other sleep disorders, such as restless leg syndrome and sleep apnea, may be associated with CRPS. Add to this the constant, tearing pain, which prevents deep restful sleep in itself.
My patients suffering from CRPS tell me that they wake up day after day feeling exhausted with no energy. Usually, people who suffer from CRPS feel more tired in the morning and many go back to sleep during the day to attempt to alleviate their fatigue. Also, it’s common for people with CRPS to have great difficulty focusing during the day, a symptom made worse by the fibro fog a lot of them already suffer from. While brain fog is often attributed to sleep deprivation, it is my belief that brain fog is not caused by insomnia, but rather made worse by it. The involvement of the cranial nerves, together with severe inflammation affecting the brain, are much likelier culprits.
While almost every CRPS patient under allopathic care is prescribed some form of sleep medication, these medications only treat the symptom of sleeplessness, and often poorly. If you want to restore deep sleep, it is crucial that the malfunctioning autonomic nervous system be balanced. Remember, your parasympathetic nervous system is not working correctly, and the parasympathetic nervous system controls your rest. To make matters worse, the less you sleep, the more severe your pain, which, in turn, leads to even poorer sleep.
Avoid Blue Lights (and we AREN’T talking about the police)
The color, determined by the wavelength, of the light we see sets our biological clocks, also known as circadian rhythms. In the natural environment, in caveman (and woman) days, this worked out pretty well. During the day, we see all the visible wavelengths provided by the sun: blue, violet, green, yellow, orange, and red light. This light communicates to our bodies that it’s daytime, time to shake a tail feather and be active. During this time, secretion of your “sleepy hormone,” melatonin, is decreased.
At night, melatonin is not affected by traditionally visible light, which consists of longer wavelengths—the yellows, oranges, and reds that we create through campfires or candles. Melatonin is released by your body like the sandman dishing out dreamtime sand. This allows us to get sleepy right when we are supposed to, together with a large part of the animal kingdom. Lullaby and goodnight.
However, we don’t use candles and fire at night anymore. We stare at our TV screens, which emanate blue light. We work on our laptops (as I am doing now)—more blue light. We use our iPhones and other smartphones—you guessed it, blue light. If we wake up in the middle of the night, we can’t resist checking our email or our Facebook accounts (maybe somebody else is awake and liked our clever post about how annoying flossing is!)
Ditto iPads and e-readers. (If you are reading this at night on one of those devices, you are suppressing your melatonin as we speak. Finish this paragraph and step away from the blue light.) Our bodies associate blue light with daytime. Blue light wakes up your brain, resets your body clock, and suppresses melatonin all at the same time. The closer your face is to the device, the worse the problem.
If you own an iPad, its blue light emissions can be reduced by adjusting the brightness and switching to white on black mode at night through the “settings” feature. If not, you can now purchase blue light filters for your computer, e-reader, iPad, or smartphone. (Just Google “blue light filters.”)
Exhaustion
While most people who suffer from CRPS attribute their daily exhaustion to pain, sleeplessness or poor quality sleep, it is usually not the only reason they feel exhausted every day. Adrenal fatigue is also a likely culprit.
Each smaller than a walnut, your two adrenal glands sit on top of your kidneys. These relatively small hormone-producing glands are powerhouses, manufacturing and secreting almost fifty different hormones including adrenalin, cortisol (stress hormone that affects things like fat storage, blood sugar, and blood pressure), estrogen, testosterone, and aldosterone (regulating salt and water levels in the body). They significantly affect the function of every organ and tissue down to every cell in your body.
When these glands are not working properly, your immune system as well as your energy level will be affected. Even your mood may be affected, causing you to see the world through a rather gray lens. When these glands are malfunctioning, your health may also be severely compromised, and you will live below your optimal potential. The adrenal glands are responsible for ensuring that your body’s reactions to stress are appropriate to optimize survival, without harming the body in return. For example, the adrenal glands are responsible for secreting protective hormones to help minimize allergic reactions such as swelling.
Adrenal fatigue is a syndrome where these glands malfunction or become fatigued due to working harder and longer than they were designed to do. This may happen after chronic or acute infections, after periods of intense stress such as losing a loved one, or during prolonged stress such as having a stressful job. It may also be caused by malfunctioning of the autonomic nervous system (as is the case in patients who suffer from CRPS). When the brain is “stuck” on sympathetic (fight or flight) overdrive, it is like your body is functioning while you are flooring the gas pedal 24/7. In response, these glands are frantically responding to this unseen stressful situation, for example, by pumping out adrenalin. Eventually, they become exhausted, leading to adrenal fatigue.
So, why don’t allopathic doctors generally diagnose adrenal fatigue? Doctors are only taught to look for extreme adrenal malfunction in medical school. This includes Cushing’s syndrome, which stems from too much cortisol production, or Addison’s disease, which occurs when the adrenal glands don’t produce enough cortisol. Traditionally, allopathic physicians check adrenal function by testing ACTH levels, using a bell curve to recognize abnormal levels. The ACTH test (also called the cosyntropin test, tetracosactide test, or Synacthen test) is a test usually ordered and interpreted by endocrinologists to assess the functioning of the adrenal glands by measuring their stress response to adrenocorticotropic (ACTH) hormone.
The problem with this test is that when it is interpreted, only the top and bottom 2 percent of the curve are considered abnormal, yet symptoms of adrenal malfunction occur after 15 percent of the mean on both sides of the curve. In other words, your adrenal glands can be functioning 20 percent below the mean and the rest of your body experiencing all the symptoms of adrenal fatigue, yet most mainstream physicians won’t diagnose you with an adrenal problem.
Signs Of Adrenal Fatigue
- Chronic fatigue and exhaustion (not relieved by sleep), usually worse in the morning and slightly better after 6:00 p.m.
- Decreased sex drive
- Inability to lose weight
- Tendency to carry excess weight in the belly area
- Recurrent infections and decreased immune system
- Lung problems such as bronchitis and asthma
- Allergies
- Sudden dizziness when you stand up from a lying or sitting position
- Muscle aches and weakness
- Depression, sadness, and a general gloomy outlook on life
- Salt or sugar cravings
- Swelling
- Excessive urination
- Hemorrhoids
- Feeling overwhelmed by even minor stress
- Struggling to get through the day
- Symptoms of hypoglycemia (shakiness, dizziness, sweating)
Please note that this list is not meant to replace a professional diagnosis, and that it is not all-inclusive.
How To Get Tested For Adrenal Fatigue At Home
In his book Adrenal Fatigue, which I highly recommend, James L. Wilson, DC, ND, PhD, describes three methods you may use at home to help determine high probability of adrenal fatigue.
- The Iris Contraction Test
For this test, you will need a mirror, a stopwatch (or a watch with a second hand), and a darkened room.
In a darkened room, sit in a chair in front of a mirror. Holding the flashlight at the side of your head, shine it across one eye (not into the eye). Watch what happens to your eye in the mirror. The pupil should immediately contract when exposed to the light, and stay contracted. If you suffer from adrenal fatigue, however, the pupil won’t be able to hold its contraction and will dilate. This dilation will take place within two minutes and last for about thirty to forty-five seconds before it contracts again. Time how long the dilation lasts and record it along with the date. Retest monthly as it serves as an indicator of recovery.
- The Blood Pressure Test (Also known as Ragland’s test)
In order to perform this test, you will need a blood pressure cuff (the type that does not require a stethoscope).
Make sure you are well hydrated before doing this test; otherwise it will give you a false positive. Lie down quietly for about ten minutes, and then take your blood pressure while still lying down. Then stand up and measure your blood pressure immediately upon standing. Normally blood pressure will rise ten to twenty mmHg from standing up. If your blood pressure drops, you likely have adrenal fatigue. The more severe the drop is, the more severe the adrenal fatigue you are suffering from.
- Sergeant’s White Line
This is the simplest of the home tests. With the capped end of a ballpoint pen, lightly stroke the skin on your abdomen, making a mark about six inches long. Within a few seconds, a line should appear. In a normal reaction, the mark is initially white, but reddens within a few seconds. If you have adrenal fatigue, the line will stay white for about two minutes and will also widen. Please note that if positive, this is an absolute confirmation. However, this sign is only present in 40% of people with adrenal fatigue.
Another test I recommend:
Saliva testing
Cortisol output by your adrenal glands is one of the most reliable indicators of your adrenal function and how well your body is dealing with stress. According to adrenalfatigue.org the cortisol/DHEAS saliva test measures the levels of the stress hormones DHEAS and cortisol in your saliva, and provides an evaluation of how these levels differ throughout the day.
(For more about this test, go to www.adrenalfatigue.org.) Another condition that shares close symptoms with adrenal fatigue is an underactive thyroid gland, or hypothyroidism.
Underactive Thyroid
(or why looking at a cookie makes you gain two pounds)
The thyroid gland is located in the front of the neck, just below the Adam’s apple. The two-inch gland consists of two lobes and is one of the largest endocrine glands in our bodies.
The function of the thyroid gland is to take iodine, found in many foods, such as seaweed, and convert it into thyroid hormones triiodothyronine (T3) and thyroxine (T4). Thyroid cells are the only cells in the body that can absorb iodine. These cells combine iodine and the amino acid tyrosine to make T3 and T4. T3 and T4 are then released into the bloodstream (the great transportation system) and are circulated throughout the body, where they control your metabolism. Metabolism is the conversion of oxygen and calories into energy. This is why the thyroid is known as the fat-burning gland. Every cell in the body depends upon thyroid hormones for regulation of its metabolism. In addition, the thyroid gland plays an important role in regulating your body’s calcium levels.
The thyroid gland, in turn, is controlled by the hypothalamus (a small area above the brain stem) and the pituitary gland (a small gland the size of a peanut, lying beneath the hypothalamus). The hypothalamus helps to coordinate the nervous and endocrine systems. It passes signals to the pituitary gland, which in turn helps to regulate growth, maturation, and metabolism.
When the body is in fight or flight mode, or the autonomic nervous system is activated, the hypothalamus sends signals to the pituitary to secrete several hormones. Adrenocorticotropic hormone acts on the adrenal gland to secrete cortisol, and TSH (thyroid-stimulating hormone) acts on the thyroid gland to secrete thyroid hormones.
Remember: The Nervous System of a CRPS Sufferer is Often Stuck in Sympathetic Overdrive.
The result of this response is that the thyroid gland of the patient who suffers from CRPS often stops working correctly. In addition, the patient’s immune system often malfunctions, leading to autoimmune conditions where the body attacks the thyroid gland.
Signs of a thyroid that ISN’T working:
- Fatigue
- Infertility
- Increased sensitivity to cold or heat
- Coarse, dry, scaly, or thick skin
- Constipation
- Difficulty concentrating
- Unexplained weight gain
- Carpal tunnel syndrome
- Puffiness and swelling around the eyes and face
- Hoarseness
- Muscle weakness
- Elevated blood cholesterol level
- Muscle aches, tenderness, and stiffness
- Pain, stiffness, or swelling in your joints
- Heavier than normal or irregular menstrual periods
- Thinning hair
- Slowed heart rate
- Depression
- Impaired memory
- Frequent urination
- Impotence
- Brittle nails
- Poor exercise tolerance
- Panic attacks
- Anxiety
How to Get Tested for a Sluggish Thyroid
- Have both T3 and T4 tested
It is very common for CRPS patients to exhibit many of the symptoms listed above, and test negative for hypothyroidism (sluggish thyroid) when their blood is tested by their allopathic doctor. It doesn’t seem to matter if you are exhibiting all of the classic signs of hypothyroidism; if the test indicates that your thyroid is normal, your doctor will typically agree with it. Doctors can be stubborn and old-fashioned like that. It is up to you, the patient (and the person who cares about your body and health the most), to inform yourself about your symptoms, the tests available to you, the tests needed in your case, and the reasons you ought to have these tests.
- TSH: The old guard’s way
The TSH (thyroid stimulating hormone) has become the “gold standard” of thyroid function. When most doctors do a thyroid test, they measure your TSH and decide, based on the test result, whether you have a thyroid problem or not. The typical reference ranges (the numbers below and above which the tests are considered abnormal) are too broad to catch minor fluctuations of the thyroid that may still be symptomatic. Also, these tests are, of course, generalized and do not consider individual differences in physiology.
Even if doctors go a step further, beyond just testing the TSH, and look at your free T4, they will typically not look at your T3 levels. This way, there is no way of knowing if your body is properly converting the T4 it makes into T3. (T4 is the inactive form of thyroid hormone. It must be converted to T3 before the body can use it). This conversion can be decreased because of inflammation or high cortisol levels. Often, regardless of your TSH testing normal, your T3 will be low, resulting in symptoms.
The TSH does not reflect the whole body, but only the function of your brain tissue. According to an expert in the treatment of the thyroid gland, David M. Derry, MD, PhD, thyroid metabolism is controlled locally in the tissue by each organ in very individual and distinct ways. The brain has one mechanism for controlling the amount of thyroid available to the brain, but it is different from that used for other tissues such as the liver. There are many mechanisms by which each tissue controls the amount of thyroid hormone it needs. When TSH is tested, that only reflects thyroid metabolism in one of your organs: the brain.
Additionally, monitoring only the TSH levels of someone undergoing treatment for a sluggish thyroid is also going to lead to under-treating the patient. The pituitary cells are the most sensitive cells in the body when it comes to circulating thyroid hormone. Therefore, if your doctor treats hypothyroidism by following the TSH and trying to make it normal, the pituitary cells are happy, but the rest of the body may not be getting nearly the amount it needs. (For more information, please research the work of Dr. Derry.)
- Thyroid Antibody Test
If you suffer from CRPS, you should ask your doctor to include the thyroid antibodies tests to detect autoimmune disease, due to the fact that the immune system of a CRPS patient is usually not functioning optimally and autoimmune conditions in this group are common.
- Reverse T3
(also known as triiodothyronine)
When your thyroid is healthy, it produces several hormones. These include T1, T2, T3, T4, and RT3 (reverse T3). T4 is a storage hormone that converts into a more active hormone, T3, as needed. Sometimes, the body just needs to get rid of excess T4, and it then converts T4 into RT3. This is mostly done by the liver. Roughly 40 percent of T4 is converted into T3 and 20 percent into RT3. However, if your body is stressed, which results in high cortisol and low adrenals, the conversion into RT3 is sped up to convert about 50 percent of T4 into RT3. This results in low T3 levels, which, as you probably can guess, are not good. Therefore, we suggest that you also get tested for RT3 (reverse T3), especially if your other thyroid tests are inconclusive.
- The Temperature Test
It is well known that a slow metabolism is a very common sign of sluggish thyroid glands. Your metabolism will directly affect your body temperature. Therefore, taking your temperature may be an important clue if you suspect that your thyroid gland is underactive. However, please note that this test is somewhat controversial in its accuracy and should not be used as a standalone diagnostic tool.
The temperature of an adult with a healthy thyroid and a healthy metabolism is (on average) 37.0 degrees Celsius or 98.6 degrees Fahrenheit. The best time to measure this is around 3:00 p.m. If you take your midafternoon temp and find it in the low 98s or even in the 97s, you have been given a strong clue that you may have an underactive thyroid.
Another good time to take your temperature is in the morning before you get out of bed. A normal morning basal temp should be between 97.8 and 98.2. If it’s higher, you may be hyperthyroid, and if it’s lower, it is possible that you have a sluggish thyroid. You may use the armpit temperature for ten minutes, but taking your oral temperature is just as effective. Be sure to add 1/2 degree to your oral temperature when comparing to the values above.
Is Your Thyroid Slow or Your Adrenals Low?
(Or both?)
If you suffer from CRPS, it can be very difficult to tell whether you have tired adrenal glands or a slow thyroid gland. Telling the two apart can be a tricky business indeed. To further complicate matters, one will affect the other, and therefore, you may suffer from both. If you suspect either of these conditions, you really should get tested for both. However, I want to mention some of the most common symptoms more unique to each condition.
Please note that this list is merely meant to serve as a guide. It is not all-inclusive and should not serve as a definitive diagnostic tool.
We have discussed in depth what autonomic dysfunction does to your body. In our other blogs we examine why your autonomic nervous system is on the fritz and why the Vagus nerve of CRPS patients malfunctions.
| Tired Adrenals | Low Thyroid |
| Weight gain around the belly areaTemperature fluctuates
Hair fine and sparse Nails thin and brittle Sunken eyes Skin dry Full eyebrows Retains fluids Ragland’s blood pressure test positive Trembling “Smoothed out” fingerprints |
Generalized weight gainTemperature fairly steady
Hair coarse and sparse Nails normal or thick Skin around eyes puffy Skin oily or moist Sparse eyebrows outer 1/3–1/4 Fluid retention normal Ragland’s test negative No trembling Normal fingerprints |
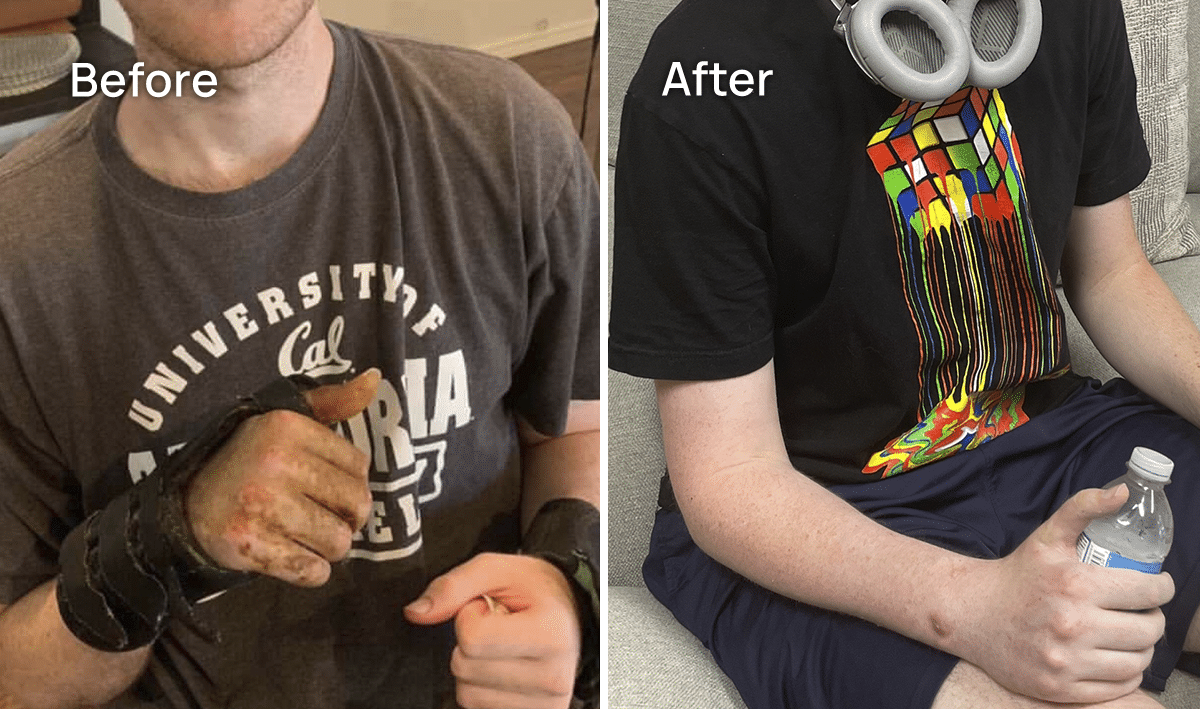
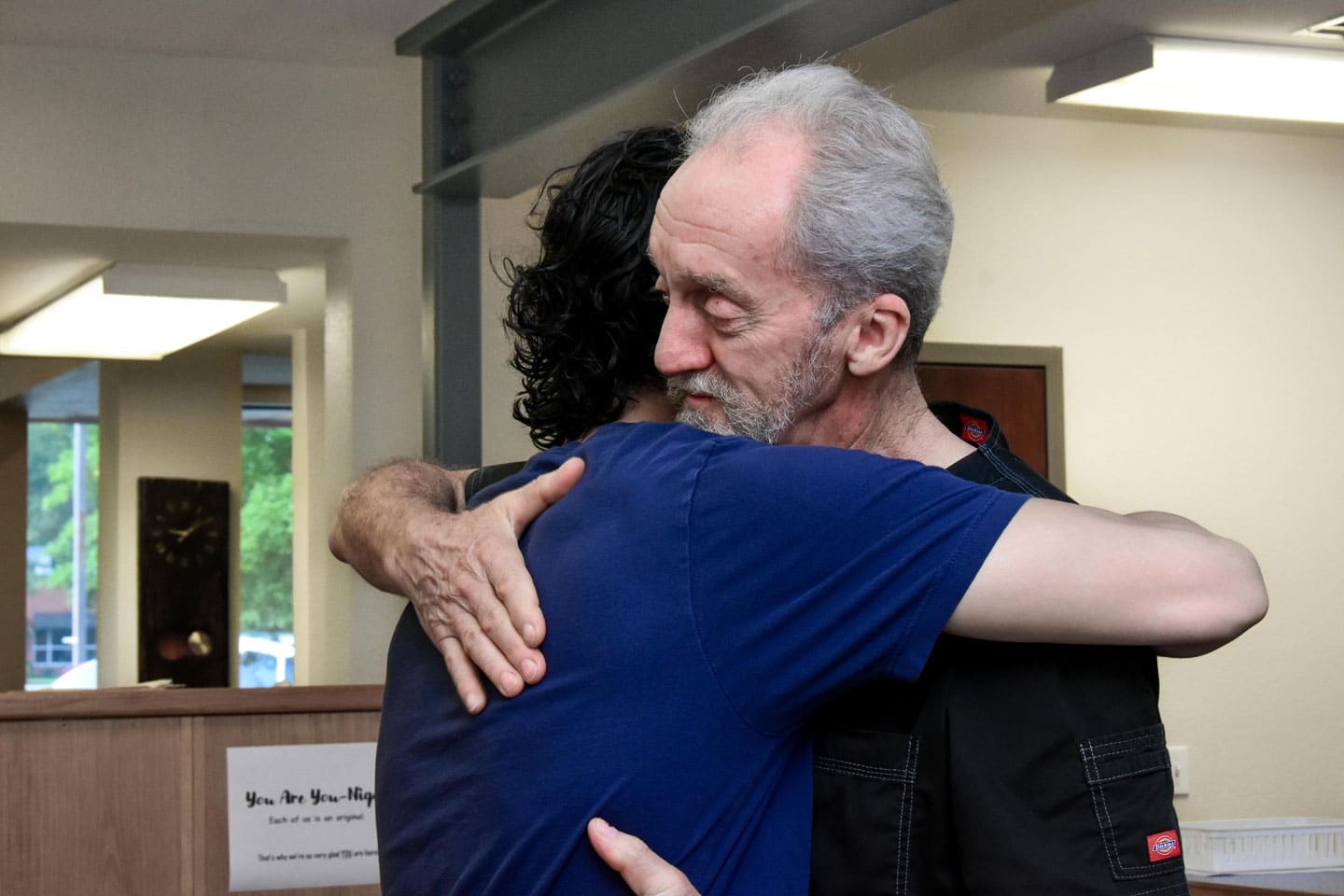
The Spero Clinic
If you or your loved one is suffering from CRPS, there is hope. Our treatment methods have helped patients enter remission after years of going through deliberating pain from CRPS. Contact us today to learn more.